Subunit Vaccine Production in CHO cells: Development of an Efficacious Ebola Virus Vaccine Candidate
Authors

Florian M. Wurm PhD, Prof. Emeri.
Chief Scientific Officer, Founder

Divor Kiseljak PhD
Director of Process Science
20th April 2020 | Last updated: 3rd August 2020
The unprecedented events tied to the COVID-19 coronavirus pandemic have underscored our vulnerability to pathogens and the importance of vaccines.
As governments implement policies to limit the spread of SARS CoV-2 by closing borders, setting curfews, and limiting social gatherings, the scientific community is working together to develop vaccines and treatments.
Looking historically, the development of a vaccine is a lengthy process.
The developed products often require stringent storage condition and specific transportation requirements.
One example of this is Merck's Ebola Zaire vaccine, Ervebo (rVSV-ZEBOV). The vaccine took years to develop, but has a short shelf-life and must be transported at -80° Celsius. These properties make the vaccine non-ideal for emergency use in sub-Saharan Africa.
Another complicating factor is that ebolavirus outbreaks are few and rare. Because of the high complexity of a virus vector-based formulation, the Merck Ebola Zaire vaccine is difficult to produce, and its limited shelf-life make it expensive to stockpile.
Nevertheless, this was the only vaccine to control outbreaks. It was first used in the Democratic Republic of Congo (DRC) during a 2018 Ebola outbreak in the Équateur province.
Just recently, in March 2020, the WHO declared the end of the Ebola Virus Disease (EVD) outbreak. This is a major victory.
However, the WHO states that there is "still a high risk of re-emergence of EVD, and a critical need to maintain response operations".
In 2017, ExcellGene and fellow members of the Pan-Ebola Vaccine Innovative Approach (PEVIA) consortium embarked on a mission to approach the development of an Ebola vaccine from a different angle.
In the following paragraphs, we describe an approach to develop safe vaccine candidates by using the strengths of knowledge-based antigen design and construction, followed by high throughput protein variant screening and coupled with the manufacturing of antigen in Chinese Hamster Ovary (CHO) cells.
We expected that this method could provide kilograms of easily manufacturable antigen product along with well-established, derisked pathways to regulatory approval.
Choosing the appropriate vaccine type and production platform
So we need to develop a stable, cost-effective vaccine that is easy to produce. Which type of vaccine best suits our needs?
We opted for a protein subunit vaccine.
Subunit vaccines are proteins or peptides, providing a safe alternative to live-attenuated bacterial or viral vaccine preparations. Usually, very small quantities of these are needed to generate cellular immune responses and neutralizing antibodies.
As a production platform, we chose to use chinese hamster ovary (CHO) cells, the workhorse of the Biotech industry.
Finding the target protein and ensuring it is efficiently produced
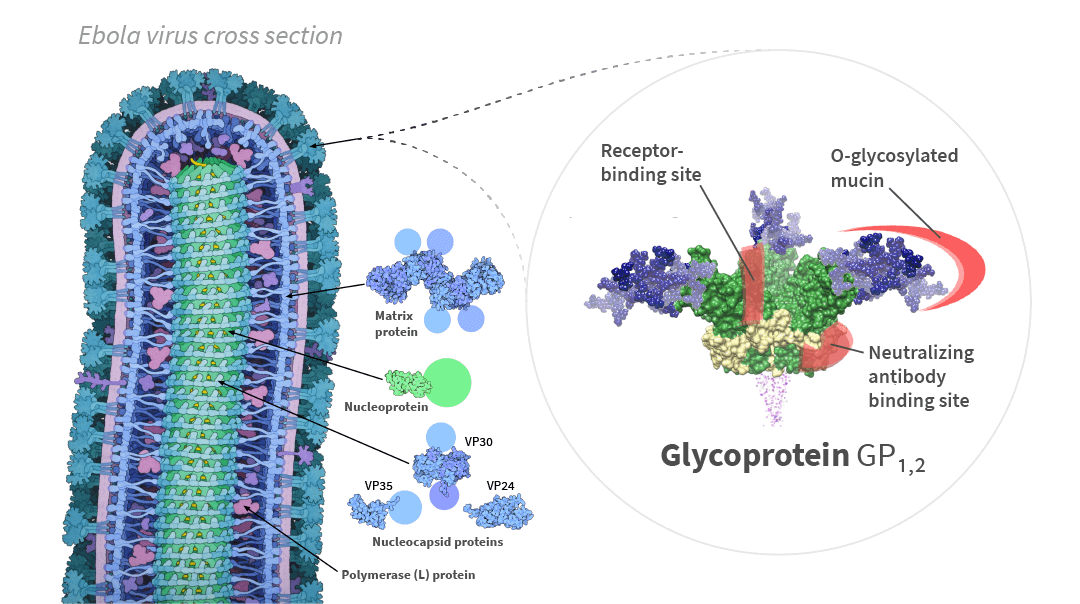
We decided to focus on the most immune-stimulatory part of the Zaire ebolavirus (EBOV). This part, called the surface glycoprotein, or GP1,2, covers the entire surface of the Ebola virus and mediates the entry of the virus into the cells of the host (See Figure 1).
Cross-sectional structure of the Ebola virus particle, and structure of the glycoprotein GP1,2 in its trimeric form [1]. Pale circles represent domains too flexible to be observed in the experimental structure.
Cross-section of Ebola virus particle drawn by David Goodsell from PDB files / CC BY.
When GP1,2 is made by production host cells, it integrates into the membrane surrounding the cell. This property makes it almost impossible to separate GP1,2 from the cells, which is required to efficiently produce the protein.
To solve this manufacturing problem, we engineered a modified version of the GP1,2 protein and established a stable CHO cell line that efficiently synthetized and secreted the variant GP1,2 protein into the supernatant of the cultures.
We then tested the purified GP1,2 protein for reactivity with sera (antibodies) from patients that survived an ebolavirus infection. The response was clearly detectable but was unfortunately too low for it to be produced as a subunit vaccine (data not shown).
Optimizing immune reactivity of the target protein
To improve the immune reactivity of the secreted GP1,2 protein, we decided to modify the protein. And to save time, we decided to design, produce and test many different versions of the protein in parallel, by high throughput screening.
One such change was the addition of a trimerization domain, to induce the formation of clusters of the GP1,2 protein. This trimeric arrangement mimics the natural state of GP1,2 on the surface of the Ebola virus (See Figure 1). Other modifications were introduced as well and constructed as individual variants and as combinations of several.
We designed and produced a total of 28 versions of GP1,2, in a matter of weeks.
All variants were tested for reactivity with the Ebola virus survivor sera. The tests clearly showed that addition of the trimerization domain and other modifications of the protein sequence increased the reactivity of the GP1,2 protein, as seen in Figure 2.
Obtaining high production yield for a cost-effective vaccine
From the experiments with the Ebola virus survivor-sera, it became clear to us that the trimeric versions of GP1,2 would be a better candidate for the production of a subunit vaccine against Ebola virus.
The problem, however, is that the production-yield of Trimer version was much lower than that of the wildtype monomeric version (15 times lower - see Figure 3). This meant that the resulting vaccine would be expensive to produce.
In an effort to solve this problem, we selected five stable cell lines (clones) that expressed acceptable quantities of this version. We then optimized each of these clones for high yielding protein production. Figure 4 shows the production yields of 180 bioreactor runs.
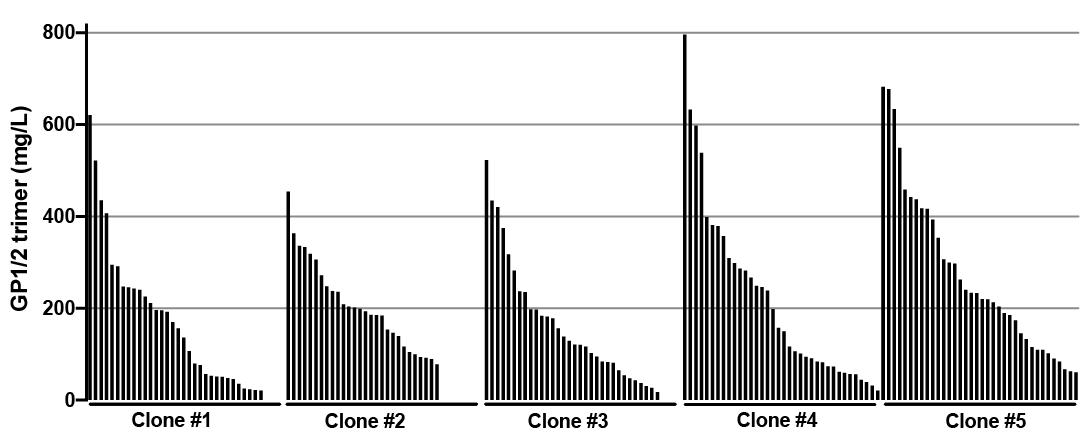
Relative yield of trimeric versions of GP1,2 from 180 bioreactor runs with five different clones of CHOExpress™ using different media and feeds
By selecting the most productive clones of CHOExpress™ host cells and by optimizing the process conditions, we were able to increase productivity by a factor of ten (from 77 to > 800 mg/L).
Does our engineered protein protect animals from Ebola virus infection?
Next, we formulated an experimental vaccine by mixing the purified protein with Freunds’ complete adjuvant to enhance the immune response to the protein.
This vaccine was then injected into the leg muscle of fifteen mice. Four weeks later, the mice were infected with Zaire ebolavirus. We monitored the mice over the course of eighteen days for clinical symptoms.
High efficacy of our ebolavirus subunit vaccine in mice
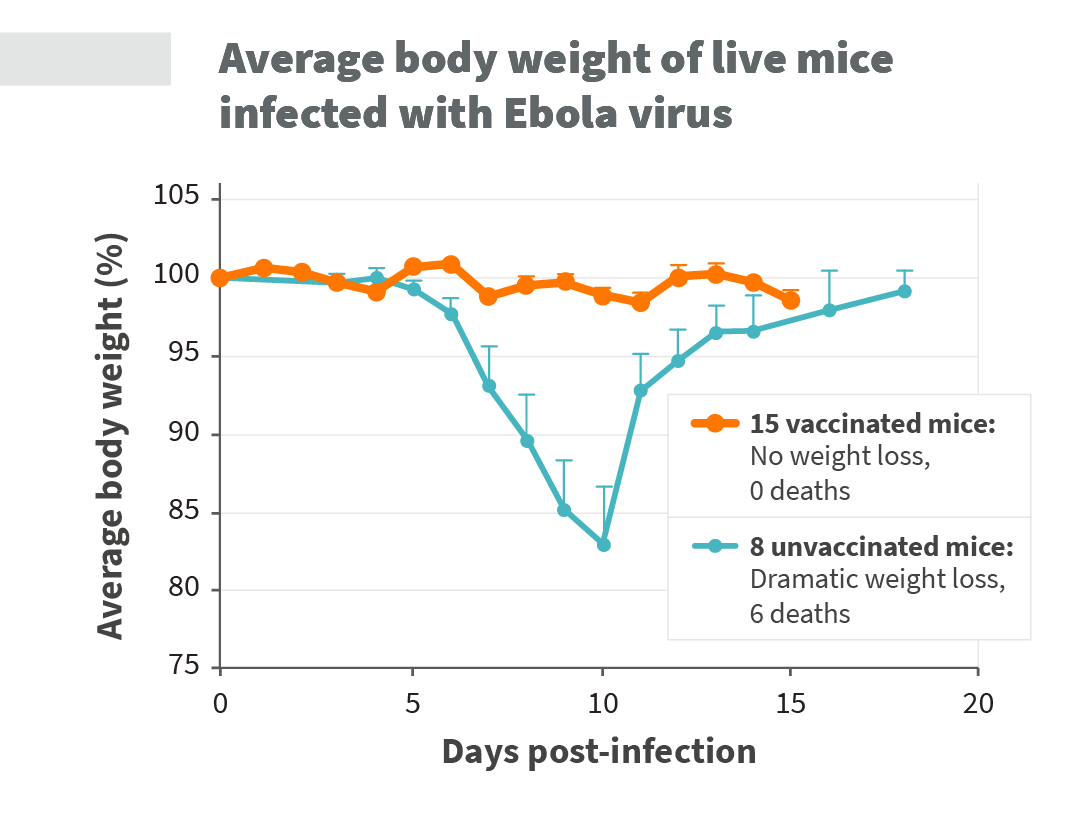
All of the non-vaccinated mice got very sick, showing extensive loss in body weight caused by loss of body fluids. Over two-thirds of the unvaccinated mice died within ten days after infection with ebolavirus (see Figure 5 and Figure 6).
In contrast, all vaccinated mice survived the challenge with ebolavirus. On top of this, the vaccinated mice did not develop any Ebola virus symptoms and retained normal body weight.
These results were provided by our fellow collaborators at the Bernhard-Nocht-Institut für Tropenmedizin in Hamburg, Germany.
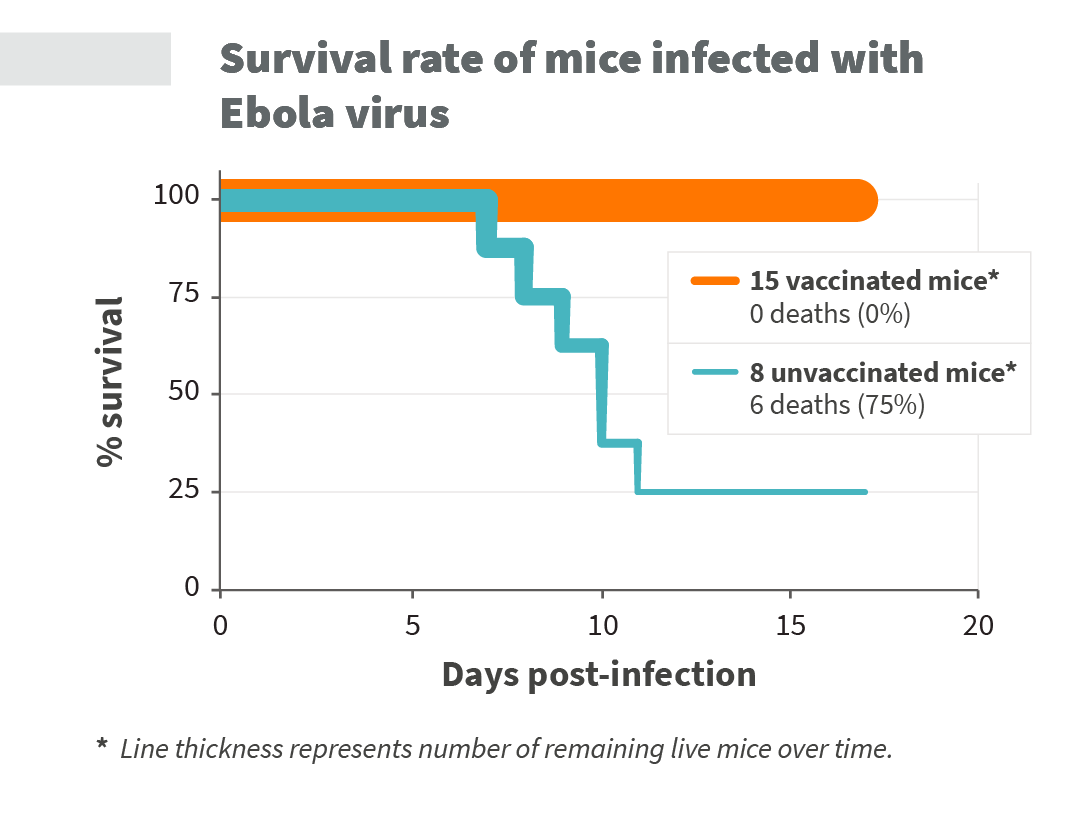
Survival rate of Ebola virus infected mice over time. The thickness of the line indicates the number of surviving mice for each timepoint.
Spurred by these promising results, ExcellGene is now moving forward towards production of the subunit vaccine candidate under cGMP.
The PEVIA consortium plans to start a Phase 1 clinical safety-study with this vaccine. During this study, healthy volunteers will be injected with our experimental ebolavirus vaccine
Our vision for a world without Ebola virus
Based on the vaccine production yields presented above, it is possible to produce millions of doses within weeks, using a standard mammalian cell-based production facility equipped with large-scale bioreactors.
The subunit vaccine described here would not only be cheap - it could probably be stored for years, and could be transported at room temperature.
We envision this vaccine to be stockpiled by governments and stored by local hospitals, so that it is available immediately in the event of an outbreak. It would even enable vaccination programs for entire populations within areas that are at risk for Ebola virus infection.
Lessons learned during our Ebola virus vaccine development project
Throughout this project, we have placed great importance on the ideal virus vaccine candidate being cost-effective, highly manufacturable, easy to transport and resilient in storage.
We believe that subunit vaccines are an effective approach to all of these challenges, especially when making full use of the strengths of protein engineering, cell line generation and process optimization.
About the authors

Florian M. Wurm PhD, Prof. Emeri.
Chief Scientific Officer, Founder
Dr. Florian Wurm is our co-founder and Chief Scientific Officer. As Professor of Biotechnology at the Swiss Federal Institute of Technology in Lausanne (EPFL) for 20 years (1995-2015) he and his students contributed highly relevant insights into the production of recombinant proteins in cultivated mammalian cells. At Genentech Inc., he was among the scientists to generate manufacturing processes for the first pharmaceutical proteins made in Chinese Hamster Ovary (CHO) cells, for which he is now considered an international expert. He has co-authored over 250 publications.

Divor Kiseljak PhD
Director of Process Science
Dr. Divor Kiseljak is our Director of Process Science. He coordinates all client projects and manages various teams covering work from DNA to protein product delivery. He joined us in 2012 as a Process Scientist after having obtained his Dr. es. Sci. (PhD) from the Swiss Federal Institute of Technology (EPFL), to further ExcellGene’s expertise in transient gene expression which was part of his doctoral work.
Divor was the scientific leader for the Ebola project. The rapid conversion of different Ebola GP1,2 constructs into purified protein was largely based on his work. He grew up in Croatia and obtained a Masters’ Degree in Molecular Biology from Faculty of Science at University of Zagreb. Through his publications, he has significantly contributed to the understanding of mechanisms and barriers for transfected DNA to be converted into high protein yields in cultivated mammalian cells.
Point of contact

Joeri Kint PhD
Chief of Business Development
Acknowledgements
We would like to express our thanks to our fellow PEVIA collaborators for their great work, as well as the Innovative Medicines Initiative, the European Union’s Horizon 2020 Research and Innovation Programme and the European Federation of Pharmaceutical Industries and Associations for their support, and for allowing this project to happen.
We also thank the Secretariat for Education, Research and Innovation (SERI) in Bern, Switzerland, which provided funding to the research group of Prof. François Spertini at the Cantonal University Hospital of Vaud and also supported the work at ExcellGene.
- Innovative Medicines Initiative (IMI)
- European Union’s Horizon 2020 Research and Innovation Programme (H2020)
- European Federation of Pharmaceutical Industries and Associations (EFPIA)
- Assistance Publique Hopitaux de Paris, Paris, France
- Bernhard-Nocht-Institut für Tropenmedizin, Hamburg, Germany
- Centre Hospitalier Regional et Universitaire de Lille, Lille, France
- Lausanne University Hospital (CHUV), Lausanne, Switzerland
- Centre National de la Recherche Scientifique Cnrs, Paris, France
- Commissariat à l'Energie Atomique et aux Energies Alternatives, Paris, France
- Heinrich Pette Institut Leibniz Institut for Experimental Virology, Hamburg, Germany
- Ifakara Health Institute Trust, Dar Es Salaam, Tanzania (United Republic Of)
- Istituto Nazionale per le Malattie Infettive Lazzaro Spallanzani (INMI) - Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Rome, Italy
- Istituto Superiore di Sanita, Roma, Italy
- Oligovax, Paris, France
- Universite d'Abomey-Calavi, Cotonou, Benin
- Vaxeal Research, Evry, France


This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No 116088. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation programme, and EFPIA.
Further reading
-
Large-scale mapping of the Ebola NP and GP proteins reveals multiple immunoprevalent and conserved CD4 T-cell epitopes
2020
Cell Mol Immunol, https://doi.org/10.1038/s41423-020-0455-2
An insightful paper by our collaborator Bernard Maillère. Mapping of the Ebola NP and GP proteins reveals immunoprevalent and conserved CD4 T-cell epitopes.
- Ebola: vers un nouveau vaccin? (French) 2020 Commissariat à l'Energie Atomique et aux Energies Alternatives, Paris, France
References
- The Secret Life of Viral Entry Glycoproteins: Moonlighting in Immune Evasion 2013 PLoS Pathog 9(5): e1003258. Google Scholar | CrossRef |